Nima Aghaeepour, PhD, was thrilled to be welcoming his first child, a daughter named Roya, which means “dream” in his native Persian. But before her due date, Aghaeepour’s wife was diagnosed with a serious complication, eventually requiring emergency surgery.
Ultimately, both mother and baby were fine. But Aghaeepour was curious. Could this outcome have been avoided?
Turning to AI for Answers
These kinds of questions don’t usually get an answer. For Aghaeepour, however, it was easy enough to find out. That’s because Aghaeepour is a world leader in applying artificial intelligence (AI) to anticipate risks for pregnant women and newborns.
Based on its analysis of hundreds of thousands of anonymized electronic medical records, Aghaeepour’s AI revealed the answer immediately: AI could have diagnosed his wife’s condition within eight hours of hospital admission. It took the medical team four days.
“Even at a top institution like Stanford, AI can see what doctors can’t,” Aghaeepour says.
Leveraging the power of this emerging technology, Aghaeepour is leading the charge to bring AI into the hospital. AI, he says, can serve as a trusted advisor for care providers, helping them deliver preventive therapies before symptoms even arise or choose the best treatment plan based on thousands of past successes.
“Artificial intelligence is not limited to mimicking humans—it can understand the limitations of human intelligence and supplement it,” Aghaeepour says. “By applying AI, we are able to enhance doctors’ ability to make correct decisions and offer treatments at the right time.”
Born into a family of engineers in Iran, Aghaeepour began writing code when he was 5 years old. His first research project applied machine learning to train robot soccer players, with the goal of beating a human team.
Wanting to make a more profound difference in the world, he then pivoted to medicine and came to Stanford University, where he is now associate professor of anesthesiology, perioperative and pain medicine, and of pediatrics. After stints in cancer and HIV research, Aghaeepour found his calling in applying AI to understand complications facing moms and babies.
“I found it compelling to focus on the very beginning of life, when you can make the most impact,” he says. “Interventions in the first few weeks of life can create as much as 90 more years for that person. This is in stark contrast to end-of-life care, where the value we can create is incremental.”
Aghaeepour and his team have already made unprecedented discoveries. Through in-depth analysis of biological samples, they pinpointed biomarkers in the blood and urine of pregnant woman that could predict preeclampsia—dangerous high blood pressure that can cause strokes or even death—months before symptoms emerge. In the current standard of care, treatment typically starts after symptoms appear, which is often too late to prevent health impacts.
More recently, by reviewing electronic health records of moms and babies using a machine learning algorithm, his team found that they could determine, even before birth, which infants were likely to face health issues with their lungs, brains, vision, hearing, and other parts of their body.
“With this knowledge, care teams can have the opportunity to perform the right interventions to prevent these terrible diseases from happening instead of just reacting to them,” Aghaeepour says.
AI-based interventions are already being used in the neonatal intensive care unit (NICU) at Lucile Packard Children’s Hospital Stanford, with great success.
Putting Technology to the Test
One such initiative employs AI to create nutritional supplements for NICU babies. By analyzing a baby’s vital information, AI can automatically generate a custom product with the right levels of sodium, potassium, calcium, and other nutrients. In so doing, it saves doctors the time they would spend on complex computations and removes the possibility of common errors that have grave consequences for babies.
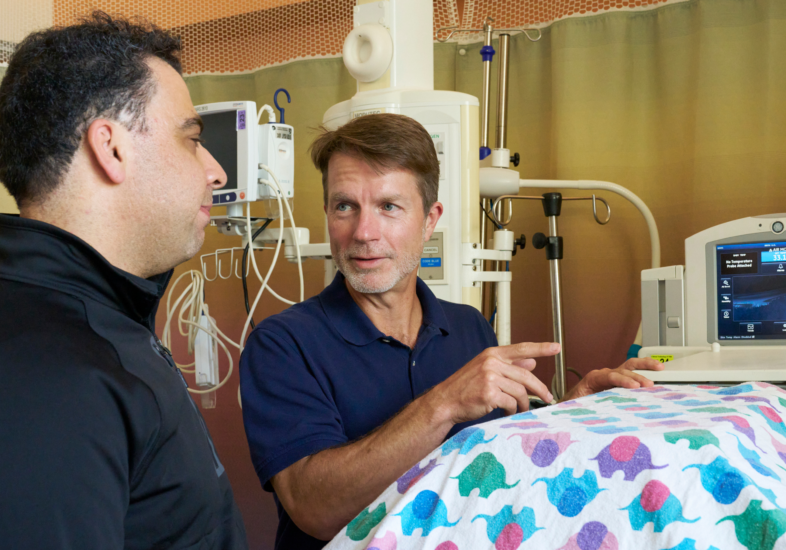
Lance Prince, MD, PhD, division chief for Neonatal and Developmental Medicine, sees incredible value in partnering with Aghaeepour to analyze and act on data about NICU patients that would otherwise disappear into thin air.
“Hidden in all those billions of data points are clues about how to take better care of kids,” Prince says. “That information is in there; we just need to figure out how to use it. And that’s what Nima and his team are magicians at doing.”
But these innovations are just scratching the surface of what’s possible, Aghaeepour says. Ultimately, he envisions a medical system in which AI seamlessly connects parents’ medical records to their child’s, predicting disease risk across generations—while also factoring in data pulled from medical records of anyone else with similar biology.
“I don’t want any aspect of health care to be driven by tradition. I want it all to be based on actual scientific data guided by AI so that, from birth, babies get the support they need, customized just for them,” Aghaeepour says. “This is borderline science fiction as far as today’s neonatology is concerned.”
Philanthropy is essential to accelerating this work, he says. “Building this infrastructure is a huge undertaking,” Aghaeepour says. “We need the support of visionaries who can see the promise of innovation long before it has become the standard way of doing things.”
If Aghaeepour’s dreams become reality, by the time his own “dream”—his daughter Roya—has a child of her own, AI will be a silent member of care teams around the world, diagnosing health challenges before they start and guiding interventions. Until that day arrives, he continues to pursue new ways to apply AI technology to improve lives.
“I want to help ensure that every baby can reach their full potential,” Aghaeepour says. “I wake up every day in disbelief that I have the privilege of being on this amazing campus, with the ability to work on impactful problems and make a real difference.”
This article originally appeared in the Fall 2023 issue of Packard Children’s News.