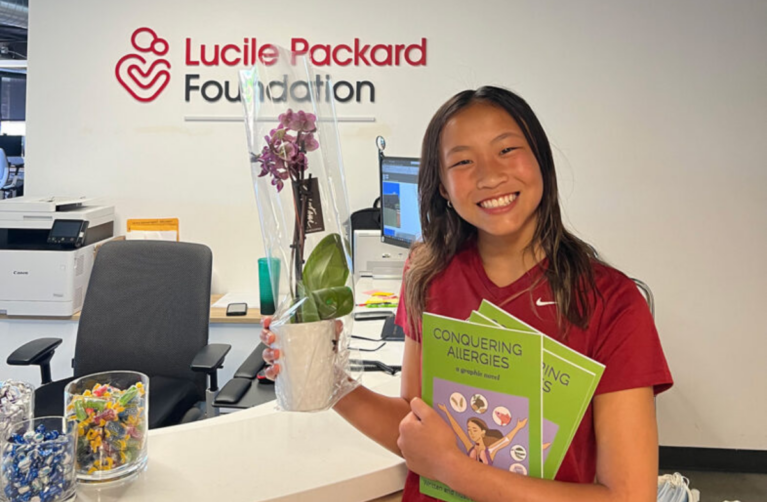
How Years of Philanthropic Support Led to a Long-Awaited Allergy Drug
“This is something that our food allergy community has been waiting a long time for,” says Dr. Sharon Chinthrajah, the acting director of the Sean N. Parker Center for Allergy and Asthma Research. This week marks a huge milestone for her team: groundbreaking research published in the New England Journal of Medicine introducing a treatment that can prevent dangerous reactions to accidental ingestions of allergy-triggering foods.
The publication presents the exciting results of a clinical trial called OUtMATCH (Omalizumab as Monotherapy and as Adjunct Therapy to Multi-Allergen OIT in Food Allergic Participants), which tested the use of the drug omalizumab (known to many as Xolair®) as a preventative treatment for food allergies. The study was funded by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institute of Health. Recognizing the significance of the study’s findings, the FDA has already approved the treatment, the first-ever drug that protects broadly against food allergy reactions.
The Impact of a New Food Allergy Treatment
The Stanford-led study’s results suggest that omalizumab (Xolair®)—currently approved for indications such as asthma and hives—has a protective effect for those with food allergies. After just four months of treatment, the majority of the study’s participants—177 children with at least three food allergies each—were able to eat small amounts of their allergy-triggering foods. In the study, Dr. Chinthrajah’s team, along with expert teams from nine sites who came together to learn from the Stanford team, used a monthly or bimonthly injection of omalizumab just under the skin. It’s a notably easy drug regimen for allergists to implement—and historically, in its use for asthma, patients have even been able to eventually self-administer at home.
The treatment has the potential to change the landscape for those living with the daily struggles of food allergies. For families who are carrying the heavy burdens of constantly monitoring food intake, this treatment offers a protective new tool in a currently limited arsenal. Dr. Chinthrajah notes the drug might be of particular interest to families of young children with severe food allergies, for it can be difficult to constantly ensure that small kids don’t put uninspected objects and food in their mouths—to say nothing of the mental toll such watchfulness can take.
The NIAID-funded study has led to FDA approval of omalizumab as a standalone treatment for food allergies, alongside avoidance. The drug now offers an alternative to oral immunotherapy (OIT), which to date has been the best available treatment for food allergies. OIT can take years and considerable effort to achieve results, especially for those with multiple food allergies, but alternatives have been sorely lacking until now.
And the possibilities are not yet fully charted. “This is just the first step,” Dr. Chinthrajah says. “[M]ore research is underway on how omalizumab can be used in combination with other approaches to treating food allergies.”
Philanthropy’s Role
The story of how philanthropy led to this breakthrough treatment is equally powerful. While the OUtMATCH study was funded by an NIAID grant, the behind-the-scenes support of steadfast donors over more than a decade was indispensable.
First, the OUtMATCH study received its NIAID grant thanks to the strength of data gathered in two preceding studies using omalizumab—and both of these earlier studies, designed by Dr. Kari Nadeau and Dr. Chinthrajah, were funded by visionary donors to the Sean N. Parker Center for Allergy and Asthma Research. According to Dr. Chinthrajah, these generous donors laid the groundwork that directly led—more than ten years later—to the OUtMATCH study’s findings and FDA approval of the treatment.
Additionally, donor gifts to the Parker Center covered uncompensated costs associated with the study. Even when a study receives prized NIH funding, much vital work happens outside the scope of the grant—and donors continue to play an instrumental role. For example, donor contributions helped fund the manufacturing facility that was integral to running the OUtMATCH study and also enabled researchers to parse out its findings.
Dr. Chinthrajah also stressed, “Every dollar has contributed to the achievements at the Center.” She remarked on how individual contributions over the years—at all levels—created momentum and fueled the research that eventually brought the Parker Center to the national stage.
Donors to allergy research are also incredibly passionate, Dr. Chinthrajah says, and a source of daily inspiration to her team. For some donors, the cause is one that is especially close to their hearts. Many families who have benefited deeply from the Parker Center’s research and care have wanted to give back however they can and contribute to a better life for other families like them. The Parker Center, established a decade ago by Silicon Valley entrepreneur and philanthropist Sean N. Parker, continues to thrive thanks to donor gifts. Today, more than 90% of the Parker Center is funded by philanthropy—an astounding level of donor engagement. Dr. Chinthrajah says, “We are so grateful for and inspired by this immense show of support!”