One big challenge of having a premature baby: the uncertainty. With good medical care, a great many preemies do very well, but some face long-term disabilities, medical complications and developmental delays, and others, sadly, die in infancy. Unfortunately, doctors can’t always tell how a baby will fare in the long term.
A new study, led by a Stanford team and conducted at 16 sites around the country, is part of the ongoing effort to change that. The researchers examined what type and timing of brain scans give doctors the greatest ability to predict preemies’ neurodevelopmental outcomes in toddlerhood. The research, published online today in Pediatrics, found that for babies born more than 12 weeks early who survive to near their original due dates, brain scans performed near their due date are better predictors than scans done near birth.
Most preemies already get at least one brain scan. That’s because national guidelines recommend that preemies’ doctors perform a cranial ultrasound seven to 14 days after birth to look for immediate problems such as bleeding into the brain. (Ultrasound is a good fit for the needs of fragile infants: Babies’ fontanelles provide “acoustic windows” to the brain, and ultrasound is non-invasive, uses no radiation, requires no sedation, and can be performed with a portable scanner brought to the bedside.) Some prior research has shown that these early scans can also give information about an infant’s risk of cognitive, motor and behavioral deficits or delays in childhood, but the predictive value of these early scans can be fairly low.
The new study examined both cranial ultrasound and MRI performed close to the baby’s due date, which is also when most preemies are ready to go home from the hospital. A lot changes in the brain during those first few weeks, perhaps explaining why later scans did a significantly better job of predicting which children would have persistent neurodevelopmental problems when the doctors checked in with them at 18 to 22 months of age.
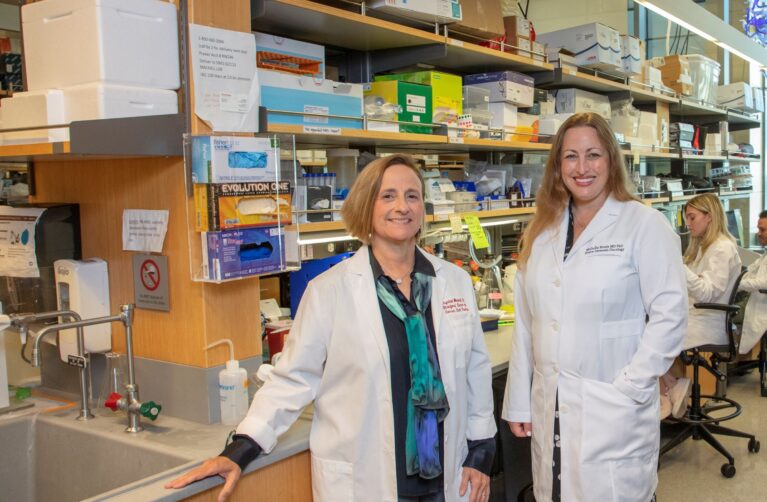
“Neuroimaging may help us understand what a child’s outcome may look like, and ultimately help us focus our attention in terms of the type of follow-up and specific interventions that could best support a child after discharge from the hospital,” said Susan Hintz, MD, the study’s lead author and a neonatologist at Lucile Packard Children’s Hospital Stanford.
An interesting detail: After late scans were considered in the researchers’ mathematical model, the results of the early scans added no significant predictive value. That doesn’t mean doctors should stop performing early scans; they still need to look for brain bleeds, for instance, and the early scans can help them plan for the baby’s hospital care. But for preemies who survive to hospital discharge, doctors should recognize the prognostic value that a later brain scan adds.
These scans still are far from perfect predictors, Hintz cautioned. For one thing, 18 to 22 months is a young age to use as an endpoint for assessing long-term neurological problems. “That just begins to tell us what the skills and challenges of a child may be,” she said. “Only as they get older and move to school age and beyond do we really get to see the full breadth of their resilience, their brain’s developmental plasticity, and their challenges, as well. Developmental outcomes are complex and influenced by multiple factors, both in the hospital and after discharge. No single test in the NICU can tell a family what the future will hold.”
The research team is still following the children who participated in this study, and plans to report again after they receive neurologic, cognitive and behavioral assessments at age 6 or 7. Ultimately, Hintz said, the team hopes their findings will advance knowledge not just of how former preemies’ brain injuries are understood, but of how such injuries can be prevented in the first place.
The research was supported in part by an Arline and Pete Harman Endowed Faculty Scholar award to Hintz from Lucile Packard Children’s Hospital Stanford. The work was also funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Neonatal Research Network.
This article originally appeared in the Scope Blog, published by Stanford Medicine.