Stanford Children’s Health Achieves Magnet Recognition
In September, the American Nurses Credentialing Center’s Magnet Recognition Program awarded Stanford Children’s Health with Magnet status as a reflection of its exemplary professional nursing practice, interprofessional teamwork, and preeminent patient care. Magnet recognition distinguishes organizations that meet rigorous standards for nursing excellence.
“We are exceptionally proud of reaching this milestone—a result of tireless dedication from our nursing and patient care leadership and everyone who delivers care at Stanford Children’s Health,” says Paul King, president and CEO of Lucile Packard Children’s Hospital Stanford and Stanford Children’s Health. “To have opened our new hospital in 2017 and now, less than two years later, meeting this extraordinary benchmark is a testament to the unparalleled quality and potential of our organization.”
To achieve initial Magnet recognition, organizations must pass a rigorous and lengthy evaluation that demands widespread participation from leadership, staff, and providers. With this credential, Stanford Children’s Health joins the global community of Magnet-recognized organizations. Just 8 percent of U.S. health care organizations have achieved Magnet status.
Autism Therapy When Used by Parents Helps Kids Speak
A new Stanford study in children with autism showed the value of teaching parents how to use everyday interactions to motivate their children to speak. The study is the world’s largest controlled trial of an autism therapy called pivotal response treatment (PRT).
The therapy works by tapping into kids’ own motivations, says pediatric psychologist and autism expert Grace Gengoux, PhD, who led the study. Children with autism often don’t make spontaneous social connections, which makes it harder for them to learn to speak. PRT teaches parents a concrete technique that takes advantage of their children’s interests—for instance, in a specific toy—to get them speaking.
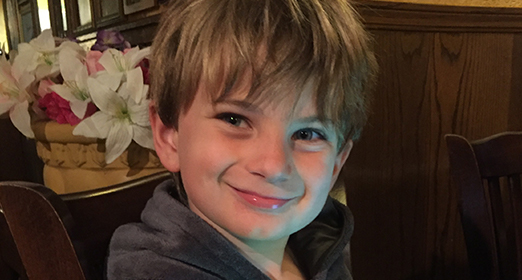
Heidi Pim of Palo Alto participated in the study with her son, James, who was diagnosed with autism and speech delays as a toddler.
“I was really worried and anxious not knowing if he would ever be able to talk,” Heidi says. She was impressed by the changes she saw in James, who was 3 at the time of the study. “I feel so grateful now to see how many words and phrases he knows. He’s able to speak clearly and socialize as well, to go up to people and ask them questions.”
Formerly Conjoined Twins Start Kindergarten
In 2016, conjoined twins Erika and Eva Sandoval underwent separation surgery at Lucile Packard Children’s Hospital Stanford. The toddlers had a 70 percent chance of survival and a prognosis with unknowns.
This fall, the girls celebrated their fifth birthdays and started kindergarten.
“With conjoined twins, you’re always cautious,” says the girls’ mother, Aida, about the risk of potential complications and new health challenges. “Like, did we hit that point yet? Have we passed that point yet? Is it safe? Now they are in kindergarten; they are 5 years old. I do see a future.”
The sisters still go to weekly doctor visits but are growing and thriving. With prosthetics and walkers, Erika and Eva live independent lives.
“It seems like such a long time ago,” says Aida. “It doesn’t feel like that was my life. But it was. It’s amazing where they were, how far they have come, and where they are going.”
U.S. News & World Report Recognizes Packard Children’s for the 15th Year
In the U.S. News & World Report 2019–20 Best Children’s Hospitals survey published online in June, Packard Children’s once again achieved rankings in all 10 pediatric specialties, with three specialties in the top 10.
Our hospital earned a top ranking for the neonatology program, sixth in the entire nation. The nephrology program is the best in California, the pulmonology program ranked best on the West Coast and eighth in the country, and our endocrinology program is the top-ranked in Northern California. The continual ranking in the top 20 of all children’s hospitals affirms the exceptional quality of care that our faculty, physicians, and team members continue to provide our patients and their families.
Remembering Christopher Dawes
Christopher G. Dawes, the former CEO of Lucile Packard Children’s Hospital Stanford, passed away on June 29 after a courageous battle with ALS. Dawes, who was 68, guided the hospital during its formative years, building it into a nationally renowned center for advanced children’s care.
He was beloved by the hospital community for his steady leadership, warm and humble nature, passionate advocacy for children’s health, and ability to listen to those around him as he implemented bold initiatives to build an outstanding enterprise.
When asked in a 2018 interview what he saw as his legacy, he said, “I am very proud of the work we do for children and pregnant women. Collectively, we have created an organization that is admired nationally and is a place that attracts great faculty and staff. We have a terrific future.”
Dawes retired in 2018 after nearly three decades with Packard Children’s.
Stranger Saves Young Patient Thanks to Social Media
Kaleb Perry has prune belly syndrome, a rare condition that is characterized by missing or severely weak abdominal muscles and problems with the kidneys and bladder. Doctors at Packard Children’s performed fetal intervention on Kaleb’s mother, Mandy, conducting five in utero surgeries throughout her pregnancy to drain Kaleb’s bladder.
Shortly after Kaleb’s first birthday, his parents learned that his kidneys were declining rapidly and that he may need dialysis. When his parents were told that they were not matches to donate a kidney to their son, they turned to the Facebook group Mandy maintained to share updates with friends and family about Kaleb’s condition. She asked followers to consider getting tested to find out if they could be a match for Kaleb’s kidney.
Within a month, Mandy received this message from Susie LeRoy, whom she had never met: “It looks like I’m going to be a good match for Kaleb.”
On May 28, Kaleb and Susie underwent surgery at Stanford to remove the kidney from Susie and place it in Kaleb. Susie was able to return home a few days later, and Kaleb was discharged from the hospital a few weeks after the transplant.
Today, Kaleb is a thriving and energetic toddler and gets together frequently with Susie’s family in the Fresno area, where they both reside.
“It’s just so surreal that this all happened and that someone would literally give a part of themself to someone to just give him life,” Kaleb’s dad, Kevin, told NBC.
Predicting Preeclampsia Risk Earlier in Pregnancy
Stanford researchers are working to develop a diagnostic blood test that can accurately predict preeclampsia prior to the onset of clinical symptoms. Affecting more than 8 million women worldwide, preeclampsia can lead to serious, even fatal, complications for both mother and baby. Clinical symptoms typically start at 20 weeks of pregnancy and include high blood pressure and signs of kidney or liver damage.
“Once these clinical symptoms appear, irreparable harm to the mother or the fetus may have already occurred,” says Stanford immunologist Brice Gaudilliere, MD, PhD. “The only available diagnostic blood test for preeclampsia is a proteomic test that measures a ratio of two proteins. While this test is good at ruling out preeclampsia once clinical symptoms have occurred, it has a poor positive predictive value.”
The team analyzed blood samples from women at various intervals during their pregnancies. They identified a set of eight immune cell responses that accurately predicted which of the women would develop preeclampsia—typically 13 weeks before clinical diagnosis.
Although their results are encouraging, more research is needed before translating them to the clinic.
New Outpatient Cardiac Care Clinic Opens
The Betty Irene Moore Children's Heart Center's newly opened outpatient clinic not only expands the capacity for patient visits—which is nearly 10,000 visits annually—it is also designed for optimal efficiency and family-centered care.
The clinic is located on the first floor of the Packard Children’s Hospital Main building and is just a short walk for cardiac care specialists to travel between the clinic and the surgery center or the cardiovascular intensive care unit. According to Robert Wenz, RN, MS, it makes for a more seamless model for cardiac specialists to treat both inpatients and outpatients without needing to leave the building.
The new spaces were designed with input from the hospital’s Family Advisory Council, a group of patient families who contribute their perspectives. One of the results of that collaboration in the Children’s Heart Center was establishing special consult rooms, apart from clinic rooms.
“Often we need to have lengthy conversations with families on their care plan or to explain a diagnosis,” says Wenz. “So we established consult rooms that offer privacy as well as comfort, with sofas and chairs, outside of the clinical care environment.”
Families of Young Heart Donor and Recipient Meet
Hana Yago was diagnosed with an enlarged heart and severe heart failure at 6 months old. By the time she was 20 months old, she relied on a ventricular device, known as the Berlin Heart, to keep her blood flowing and extend the life of her failing heart. She needed a transplant to survive.
Leo Bibler was the same age as Hana. Sadly, in late May 2016, he passed away after a seizure. His parents, Kelly and Dave, learned their little boy could save eight lives through the gift of organ donation.
Shortly before her second birthday, Hana received her new heart.
Last summer, the Biblers drove 1,200 miles from their home in Colorado to Palo Alto to meet Hana and her family for the first time. Hana, who is now 5 years old, recently celebrated her third “heartversary.” Hana’s mom, Kathleen, told the Biblers how much their son’s gift meant: “To give a kid you never knew another chance at life, it’s kind of overwhelming and beautiful, and we are so grateful.”
Dave and Kelly took turns holding a stethoscope to Hana’s chest and listening to Leo’s heart beating inside her. “That is so cool,” Dave told Hana. “You have a good heart in there.”
See the moment Hana met her heart donor’s family: supportLPCH.org/LeoandHana.
This article originally appeared in the Fall 2019 issue of Packard Children’s News.