Dr. Amanda P. Williams Explains California’s Progress and Why Urgent Action Is Still Needed
In the U.S., Black women are three to four times as likely as their white peers to die giving birth, and twice as likely to have severe pregnancy complications. It’s a major health crisis given that the U.S.’ overall maternal mortality is the highest among economic peer countries.
But there’s reason for optimism in California, where maternal death rates are the lowest in the nation. That’s largely due to a Stanford-based organization called the California Maternal Quality Care Collaborative (CMQCC).

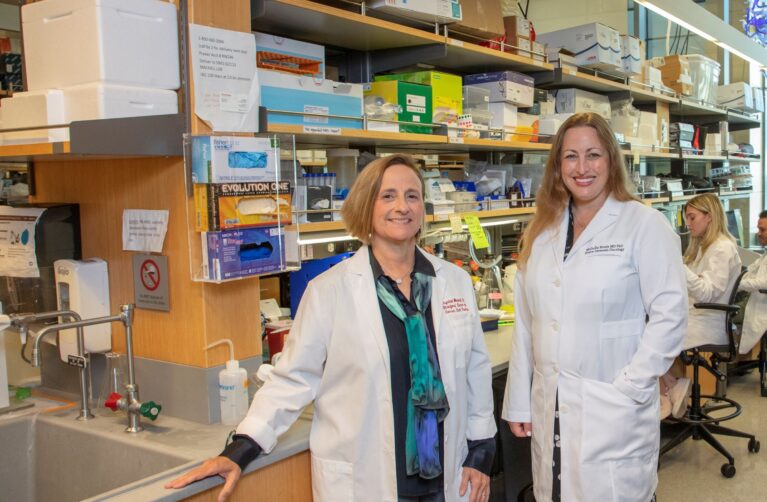
We spoke with Amanda P. Williams, MD, MPH, FACOG, clinical innovation advisor at CMQCC since 2022, about the remarkable progress and next steps in reducing disparities for Black patients. Williams, who is Black, is a survivor of a serious pregnancy complication, an experience that drives her to address racism in maternity care.
Q: What’s behind California’s success in reducing maternal mortality?
California’s maternal death rate is about half the national average. Since 2006, CMQCC has been developing targeted, measurable ways to reduce obstetric complications and deaths. We put together evidence-based policies and practices to address common complications such as hemorrhage and high blood pressure. Thereafter, we implemented multi-hospital collaboratives to share best practices and create toolkits for the over 200 hospitals statewide. We also collect and collate data to help hospitals understand their performance and outcomes, benchmarking against other hospitals in the state and national quality goals.
Most maternal deaths are preventable. By applying the same standardized approaches to more patients, we helped reduce maternal mortality statewide by 65% between 2006 and 2016, while the national rate continued to rise.
Q: Even in California, there’s still a gap in outcomes for Black patients. What is CMQCC doing next to address this?
We know that disparities are partly linked to factors such as income, education, access to care, and preexisting health conditions. However, after accounting for these factors, Black and Indigenous women still experience twice the number of complications and deaths. There must be more to the story and that X factor is systemic racism. We’re proud that the rate of preventable deaths is lower in California than elsewhere in the U.S., but it’s still unacceptably high—and way too many of these women look like me.
Your money won’t save you. In a Stanford study last year, rates of neonatal death and maternal death are higher even among the wealthiest Black moms, compared with white moms from the lowest tax bracket. Serena Williams and Beyoncé, women with seemingly unlimited funds and access to the greatest doctors anywhere on the planet, have used their platforms to publicly share their stories of birth-related complications.
We’ve addressed the lower-hanging fruit with systematic approaches to obstetric complications. Next, we need to dig into the systemic racism that has been enmeshed into the practice of American medicine, which is much more challenging to confront as well as detangle.
You’re not likely to see outright bigotry in California patient care, but we’re digging into those scenarios where implicit bias still occurs. Our data show that, even today, patients’ complaints of pain or bleeding aren’t being listened to. For women in labor and delivery, that can be a matter of life and death.
CMQCC now has multiple active projects addressing perinatal equity in California. We have launched the Hospital Action Guide for Respectful Equity- Centered Obstetric Care, an interactive resource with two purposes: First, it will help California hospital users understand the drivers of inequities in maternal care, and how and why racism, discrimination, and implicit bias are root causes of maternal inequities. Second, it provides hospital maternity teams with a sample of action-oriented, equity-centered tools and resources that go beyond implicit bias training and may translate into real change in culture and patient care.
We have also begun a statewide Learning Initiative for Supporting Vaginal Birth Through an Equity Lens. With funding from the Centers for Disease Control and Prevention, this collaborative charges us to touch every hospital in the state either through direct use of the Action Guide or participation in the Learning Initiative that brings together cohorts of hospitals to learn and grow. With NIH funding through our partnership with the Stanford Ob/Gyn Department, we are augmenting the learning initiative by analyzing the tools that create the largest impact as well as collecting qualitative data.
Q: How does your own experience with pregnancy and childbirth inform this work?
I was the chief resident in obstetrics and gynecology at the University of California, San Francisco (UCSF), and a very healthy former track athlete when I had preeclampsia with my first child in 2004. I couldn’t have had more intellectual or educational privilege, or better access to care. And yet here I was having significant complications. I was fortunate to have been at UCSF Medical Center and to have access to such tremendous care; otherwise, things could have gone very badly.
Over the ensuing 17 years I took care of thousands of pregnant patients and witnessed intimately how our medical system is not designed to support people of color. In 2022 I left my job at Kaiser Permanente to devote myself to birth equity. We have done so much in California to address maternal morbidity and mortality for common obstetric complications. Now it’s time to systematically address racism and help hospitals activate solutions.
Q: How is philanthropy advancing CMQCC’s work?
Philanthropy has played a huge role in CMQCC’s success. Early gifts from donors helped launch CMQCC in 2006—and that generosity has continued over the last 18 years. Two recent examples: a grant from the Skyline Foundation launched the Community Birth Partnership Initiative to improve the integration of midwives working in the community setting while ensuring safe transfer of care to a hospital when needed, and to enhance access to doula care. And funding from Merck for Mothers is supporting our deep dive into optimizing postpartum care for up to a full year for all birthing people.
Q: How can improvements in California make a difference for patients in other states?
People may not be aware, but one out of every eight babies in the U.S. is born in California. We make our tools publicly available on the CMQCC.org website, and we speak across the country to share our learnings with other states. If we can make things better here, things can be made better anywhere.
This article originally appeared in the Spring 2024 issue of Packard Children’s News.