Ensuring Access to Health Care for Medicaid and CHIP Enrolled Children During and Beyond the Public Health Emergency
Organization: Manatt Health Solutions
Primary Contact: Cindy Mann
Grant Amount: $150,000 for 6 months
Date Awarded:
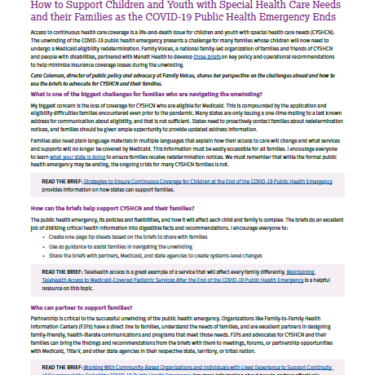
Purpose
One of the key issues facing families and policymakers as the COVID-19 pandemic transitions to an endemic issue is the impending “unwinding” of continuous coverage under Medicaid and the end to state flexibilities granted for the duration of the public health emergency. About half of all children in the US have insurance coverage through Medicaid or the Children’s Health Insurance Program. Since the beginning of the pandemic, all states have been federally required to maintain continuous Medicaid coverage for children who were covered as of March 2020. It is likely that these coverage requirements will expire in 2022, leaving states to redetermine eligibility for millions of pending Medicaid cases. There is an extremely high risk that individuals will become uninsured even though they may continue to remain eligible for coverage. This is a life-and-death issue for children with special health care needs (CSHCN). Building on previous foundation-funded work to ensure access to Medicaid services for CSHCN, Manatt will prepare a set of rapid response policy briefs on key policy and operational recommendations to help minimize insurance coverage losses for CSHCN during the unwinding. A set of topic-specific one-pagers to support state-level advocacy efforts by family leaders also will be developed. This project will be conducted in partnership with Family Voices. This partnership will encompass regular meetings to share emerging issues that will impact CSHCN at the end of the public health emergency, targeted technical assistance to support state-level advocacy efforts by family organizations, and financial support for family engagement.